GNLM – Myanmar Daily News, Myanmar Latest News, Myanmar News Today
Myanmar’s industrial product exports cross US$130M in 5 days
According to the Ministry of Commerce, Myanmar has earned a total of US$130.506 million from exporting finished industrial products within […]
Temporary intl cargo ports enable export to neighbouring countries
Shweme Port and Mottama Port from Shwepyitha Township, Yangon Region, were approved by the Customs Department as temporary international cargo […]
Belt and Road Scholarship: Myanmar’s Spring Tea Reception held in Hong Kong
According to the Ministry of Foreign Affairs (MoFA), U Han Win Naing, Myanmar’s Consul-General in Hong Kong, attended the “Belt […]
Myanmar celebrates World Immunization Week 2024
The Ministry of Health marked World Immunization Week in Nay Pyi Taw yesterday. At the event, Union Minister for Health […]
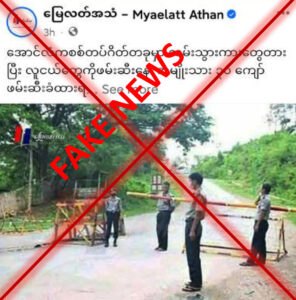
Misinformation: Over 30 men arrested at Aunglan inspection checkpoint
The malicious news media falsely posted that more than 30 men were arrested at the Aunglan inspection checkpoint of Magway […]
Myanmar’s industrial product exports cross US$130M in 5 days
Pantanaw new long chilli price declines to K3,600 per viss
Palm oil reference price spirals down again in Yangon market
Myanmar celebrates World Immunization Week 2024
Investors Club’s 31st Anniversary held in New Delhi
Central Committee on Copyright meeting 1/2024 held
No Use
By Kyaw Myint Tun (Paris) For ease of reference, let’s continue to refer to these hypocrites, who descend from their […]
Why Not Read Novels?
By Hu Wo (Cuckoo’s Song) According to Oxford, novels are stories long enough to fill a complete book, in which […]
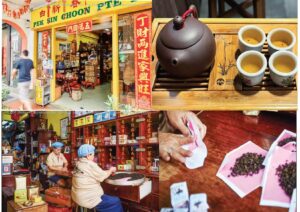
Journey Through the Timeless Tea Legacy
By Yin Nwe Ko Tucked away in a heritage shophouse on Mosque Street in Singapore’s Chinatown, Pek Sin Choon is […]
Sustain health of mother earth with plastic waste management
T he Earth serves as a vital habitat for all forms of life, encompassing humans, animals, plants, and various objects. […]
Shakespeare’s Enduring Legacy
S hakespeare was a famous writer. He wrote many good and winning plays. He created many attractive plays. When I […]